
Pain scores were collected at the initial visit (timepoint 0), and at four subsequent time points (three, seven, 21, and 42 days postinjury) via an automated online text messaging system. Permission for the evaluation was granted by the R&D department of Alder Hey Children’s Hospital as a service evaluation. If the child had attended the clinic after 24 hours, the child was asked to recall how much pain they had after the injury to produce timepoint ‘0’.
Parents were taught to read the pain scale instructions to their child to enable follow-up at home, inviting the child to select the face that best depicted their level of pain. Patient consent and study information, including a copy of the Wong Baker Faces Pain Scale, 8 was issued to the patient at first contact.
#BUCKLE FRACTURE TRIAL#
There was evidence that the patient would be unable to adhere to trial procedures or complete follow-up, such as cognitive impairment or no access by parents to a mobile telephone. Patients were eligible for the study if they met the following inclusion criteria: It has been validated as a self-reporting tool for use among children over three years of age, including in the paediatric emergency department setting, and has been identified to be an excellent measure of pain when estimating the effect of treatment intervention.
#BUCKLE FRACTURE SERIES#
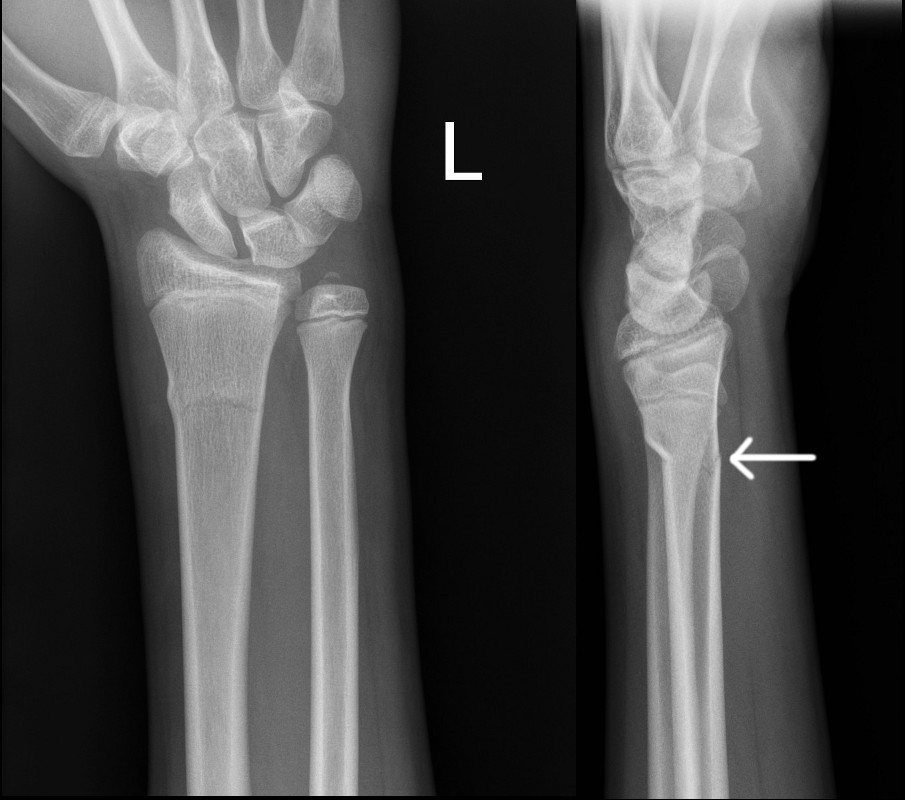
The primary outcome used was the Wong Baker Faces Pain Scale, 8 a validated self-reported tool, and an ordinal assessment of pain outcomes using a series of six facial expressions to illustrate the degree of pain intensity. All children were immobilized in a rigid wrist splint, with the advice that they should wear the splint for three weeks and then remove it, but to avoid sports for a further three weeks thereafter. Patients were either seen in the accident and emergency department, whereby patients were discharged at initial contact, or at the orthopaedic fracture clinic, where patients were referred from neighbouring minor injury units. Patients with torus fractures of the distal radius were identified on presentation to Alder Hey Children’s Hospital over a six-week period (November to December 2016). This study informs the feasibility of a randomized controlled trial by assessing the variation in pain scores, the variation and duration of symptoms, and engagement with an innovative text service as a data capture tool.

The NICE review, which was unable to advise the best form of immobilization owing to the poor quality of the available evidence, and the recommendation that a trial of treatment interventions was necessary. The recent National Institute for Health and Care Excellence (NICE) non-complex fracture guidelines made recommendations on the management of these injuries, 1 advocating that they should not be immobilized in a plaster, and that they should be discharged from the emergency department without a subsequent follow-up. However, there is growing evidence to support the absence of complications in these fractures, with widespread acceptance that patients may safely be discharged at diagnosis, 2- 4 and that rigid immobilization may not improve pain control but will unduly restrict function. cast/rigid splint) argue that this maximizes pain relief, and minimizes the occurrence of complications, i.e.
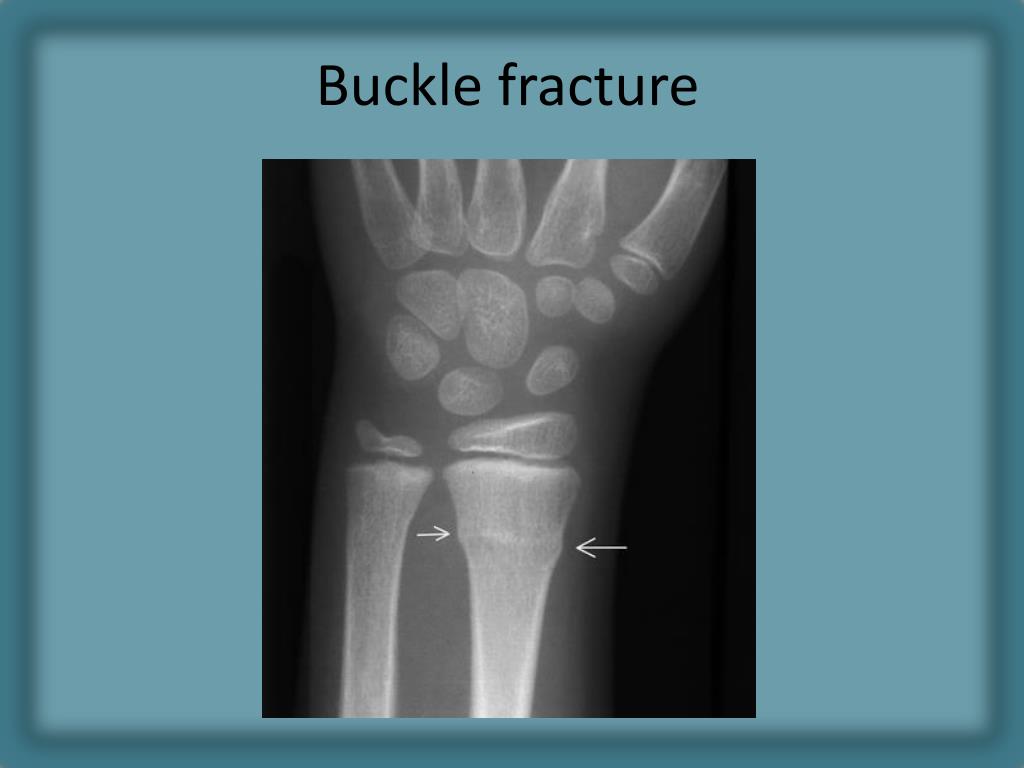
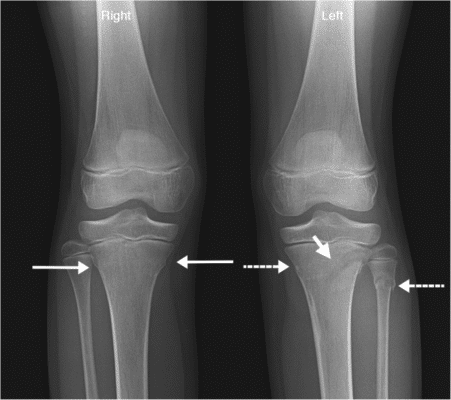
2- 7 The proponents of rigid immobilization (i.e. The variation in practice has arisen from a longstanding doctrine of rigid cast immobilization for fractures, 3 tempered with newer evidence to suggest that simpler treatment methods are frequently as effective, or perhaps even more effective. Treatment varies from soft bandaging, to the use of a removable splint, and rigid plaster cast immobilization. There is considerable variation in the management of this injury. Torus fractures are very low risk injuries for complications or deformity in the skeletally immature, and these fractures universally heal well. 1 They occur when the radius and/or ulna bone buckles, such that there is cortical deformation but no break in the cortex. Torus fractures of the forearm account for an estimated 500,000 emergency department attendances a year in the UK.


 0 kommentar(er)
0 kommentar(er)
